The start of a new year brings new members with new health plan names and member ID cards. If your practice is contracted for our Medicare or Health Insurance Marketplace products, remember that members may mention these health plan names when they make appointments::
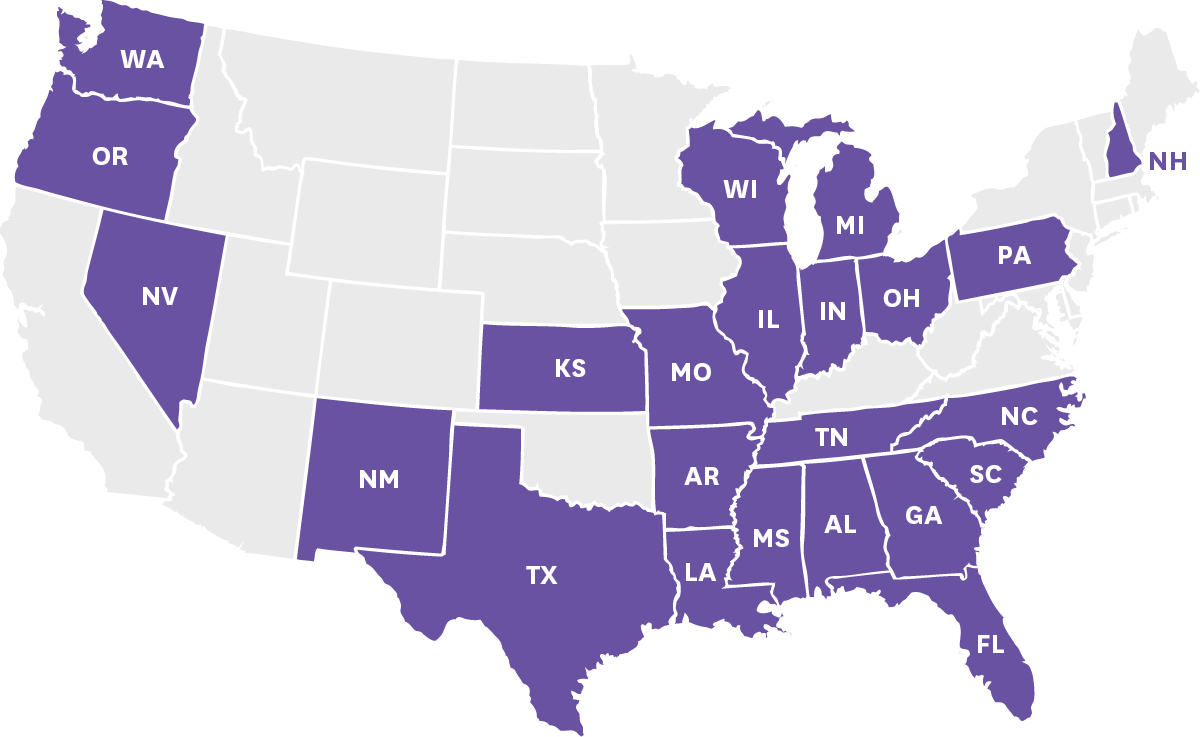

AZ, FL, GA, IN, KS, LA, MO, MS, NM, NV, OH, PA, and TX

AR, AZ, FL, GA, IL, IN, KS, MI, MO, MS, NC, NH, NV, OH, PA, SC, TN and TX

AL, FL, IL, IN, KS, MI, and TN

OR

OR
Remember, before providing services to any member, it is important that your office:
Envolve Vision providers should not bill Medicaid and Medicare members for services that include fees to cover the costs of personal protection equipment (PPE) such as infection control fee, biohazard fee, miscellaneous fee, etc.
As a reminder, Envolve’s Utilization Management clinical criteria is available by logging into Eye Health Manager and clicking on Provider Resources, then Policies and Procedures, and then Utilization Management. To request online access, visit the Request Access page or call the Customer Service Number for your market. You may also request copies of our clinical criteria by calling the Customer Service number for your market.
For your convenience, all eligible ICD codes can be found on Envolve Vision’s website at
For Texas providers, eligible ICD codes are available by logging in to Eye Health Manager and viewing your provider manual.

Envolve Vision is committed to improving the health of our community by helping people with diabetes lead healthier lives. Because of your vital role in patient health, we are asking for your assistance by facilitating preventive care through annual diabetic eye exams and reporting of exam findings.
Routine retinal evaluation is recommended to reduce the risk of diabetes-related blindness. While exams do not require prior authorization, please be sure to adhere to Envolve Vision’s clinical policies regarding medical necessity.
Visit envolvevision.com/logon to view medical necessity guidelines and verify member benefits and eligibility.
Please reference plan specifics and applicable billing guidelines when selecting the most appropriate CPT code for services rendered.
Using these codes may help reduce the need for medical record reviews.
*Note: Select health plans offer reimbursements for CPT II codes. Please consult your plan specs for details. If applicable, when submitting CPT II codes, providers must bill $10 in the claim filing to receive reimbursement.
Envolve Vision offers a Provider Education page for your convenience. Click below for:
Please verify that your office information is up-to-date – including office hours or contact information that may have recently changed. Here's how to update your information for the Provider Directory:
All eye doctors are re-credentialed every 36 months unless otherwise requested by the payor. Reminder notices are distributed three months and one month prior to the expiration of the eye doctor's credentials. Anyone who fails to re-credential may be terminated from our provider panel for any applicable products.
As a reminder, referrals from a primary care physician (PCP) are not required for a member to schedule an eye exam with any participating optometrist or ophthalmologist. If you have any questions, please call Customer Service.
Unless otherwise stated in the Plan Specifics (found in the Eye Health Manager at
envolvevision.com/logon), providers have these options to submit claims to Envolve Vision via the following:
Envolve Vision, Inc.
P.O. Box 7548
Rocky Mount, NC 27804
Envolve Vision strongly encourages verifying member eligibility prior to rendering services. Providers may verify eligibility through Eye Health Manager at envolvevision.com/logon or by calling Customer Service at the number provided for your market.


by Jill Scullion, OD, MBA Vice President, Health Care Services
We all know preventive health screenings and regular well-check visits are essential for catching early signs of illness and helping patients maintain good overall health. However, the social determinants of health that lower-income patients, such as Medicaid beneficiaries, face often make it difficult for them to attend regular primary care visits.
For Medicaid beneficiaries and others who struggle to get screenings or attend regular appointments, ODs are the first line of preventive care. For one, standard eye exams are very important for vision health. The CDC says more than 60 million adults in the U.S. are at high risk for vision loss. Yet of that population, only 50% have seen an OD in the past year.
Consistent eye care can have a profound impact on overall health, as many systemic diseases can be identified through changes in eye health. But an engaged Medicaid population creates a ripple of positive effects that extend beyond the individual. By engaging their Medicaid patients, ODs become better stewards of community health. The value they bring to the community is enormous: In making early treatment of disease possible, they allow health systems to allocate resources appropriately and deliver high-quality services at lower costs.
Below are three ways ODs can improve Medicaid patients’ healthcare outcomes.

For more than 30 years, Envolve Vision has partnered with vision care providers across the country to administer eye care programs that meet the needs of their members. You are among 22,000+ unique eye care providers, including independent providers and popular retail chains, within our network. Thank you for partnering with us to provide quality vision services to your patients.
